Treatment For Interstitial Lung Disease
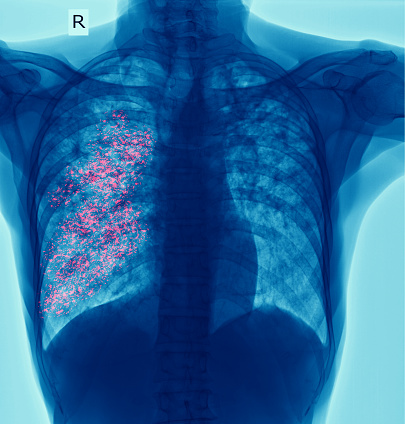
Treatment for interstitial lung disease varies depending on the type of disease. Some cases are mild and in less than 10% of patients, and in these cases, a simple chest X-ray may be all that’s needed. In more serious cases, a high-resolution CT scan may be required. Echocardiography may also be necessary to check for abnormal pressures in the left side of the heart.
Can interstitial lung disease be cured?
There are over 200 different conditions that fall under the umbrella term of interstitial lung disease (ILD). Generally, people with ILD have scarring or inflammation of the lung tissue that affects their ability to breathe. This scarring limits the amount of oxygen that can get into the blood stream. Interstitial lung disease can be acute or chronic. In severe cases, people can develop pneumonia. This is usually caused by bacteria.
Treatments for ILD include medicines to treat the symptoms of the disease. These include inhalers called bronchodilators. While these medicines are effective, they need to be taken correctly in order to prevent lung scarring. The National Asthma Council of Australia has an Inhaler Checklist to ensure that these medicines are properly used. Patients may also require surgery or lung transplant.
There is no cure for interstitial lung disease. However, treatments for the disease can improve lung function and improve the quality of life of sufferers. Unfortunately, interstitial lung disease is a progressive condition. There is no cure for it, and there are no known treatments that can reverse its progression. However, there are several treatments that can help patients cope with their symptoms and keep the disease from progressing.
How serious is interstitial lung disease?
Interstitial lung disease is a condition in which scar tissue develops in the lungs. It can be caused by a number of factors, including certain heart medications and chemotherapy drugs. In addition, some antibiotics can damage lung tissue. These include nitrofurantoin, ethambutol, and rituximab. In addition to treating the symptoms of interstitial lung disease, doctors can prescribe antifibrotics, which help protect the lung from further damage.
There are many different types of interstitial lung disease. They start with an inflammation around the alveoli, which are tiny sacs in the lungs that transport oxygen into the bloodstream. However, these diseases can affect other parts of the lungs as well. Because of this, their symptoms can be similar to those of other respiratory conditions. Some people with severe interstitial lung disease may require a ventilator to help them breathe.
Interstitial lung disease symptoms range from mild to severe, and they can vary over a long period of time. Some may last for months or years, while others worsen rapidly. The most common symptom is difficulty breathing, which is often accompanied by cough and other respiratory symptoms. The severity of these symptoms depends on the underlying cause of the disease.
Is walking good for interstitial lung disease?
There are several studies that have looked at the effect of walking on lung health. A large cohort of people with interstitial lung disease has been studied. Researchers have used the 6-minute walk test to predict survival in this patient population. It has also been used to assess pulmonary arterial pressure.
One study found that walking helped people with scleroderma lung disease improve their lung function. In addition, the study also found that supplemental oxygen improves the outcomes of exercise training. A six-minute walk test using forehead oximetry is a reliable way to assess the effectiveness of exercise training in people with this disease. Another study looked at the benefits of exercise training for people with pulmonary fibrosis.
However, patients should be aware of the risk of hypoxemia during exercise. Patients with ILD are more likely to experience dehydration than healthy people. Therefore, it is important to use a heart rate monitor while exercising to ensure that your heart is functioning properly.
Can interstitial lung disease go into remission?
Interstitial lung disease, or ILD, is a class of rare pulmonary disorders. Some are inflammatory while others are fibrotic, and many are a combination of both. ILDs vary in their clinical course, with some going into remission or stabilizing, while others progress to death. Most patients have symptoms that affect their ability to live a normal life, including coughing, fatigue, and dyspnea.
The main difference between patients with hypersensitivity pneumonitis and those with usual interstitial lung disease is the presence of pulmonary fibrosis. Researchers examined the histopathology of 16 autopsy cases of patients with these conditions. In addition, they studied patients with both chronic hypersensitivity pneumonitis and lung cancer.
Is interstitial lung disease a critical illness?
Interstitial lung disease is a progressive condition that destroys the lung tissue. It results in scarring that makes breathing difficult and can cause life-threatening complications, including lung infections and respiratory failure. Symptoms vary from mild to severe and can come and go rapidly. They may include coughing up blood or mucus, chest pain, shortness of breath, and increased body temperature.
Because of its many potential causes, it is difficult to accurately diagnose ILD. Obtaining an accurate diagnosis is essential to obtaining further information about the condition and treatment options. The University of Michigan Interstitial Lung Disease Program is dedicated to ensuring accurate diagnoses. Its team of experts has studied the diagnostic methods used for this illness and has developed a standard multidisciplinary approach to the diagnosis. In addition, they are members of an international task force that is revising the diagnostic criteria.
The diagnosis of ILD can be difficult and requires input from different specialists, including pulmonologists, radiologists, and pathologists. Multidisciplinary case conferences are necessary to obtain a proper diagnosis. Usually, the diagnosis is made through a thorough history and physical examination, including a stethoscope. The doctor will also examine the skin and joints. In some cases, a diagnosis can be made through a biopsy.
How painful is interstitial lung disease?
If you’re wondering, “How painful is interstitial lung disease treatment?” there’s no single answer. The treatment varies from person to person, but there are some common factors that you need to be aware of. The doctor will need to administer medications that will control inflammation. The treatment will help your condition and give you a higher quality of life.
If you have a history of lung disease, you may consider joining a support group to share your experience. This group may provide you with coping tips and share information on new treatments. Alternatively, you can talk to a professional counselor in a one-on-one setting. Regardless of the treatment you choose, you’ll most likely be seen by your family doctor. Your doctor may refer you to a pulmonologist. He or she may perform a number of tests to diagnose your condition, including a chest CT scan and pulmonary function tests.
There are many different types of interstitial lung disease. However, they all begin with inflammation and scarring in the lungs. It makes it harder for the body to move oxygen out of the lungs, which leads to breathlessness. Patients with interstitial lung disease may feel short of breath or coughing, or they may experience symptoms of asthma or other medical conditions.
How long can you live with scarred lungs?
When you have scarred lungs, oxygen is not able to reach all of your organs. This can lead to pneumonia and pulmonary emboli. Other serious conditions can also develop with this condition, such as pulmonary hypertension, where blood pressure builds up in the lungs. People with this disorder usually live three to five years after diagnosis, but the course of the disease can be unpredictable.
There are several types of scarring in the lungs, which may be caused by a number of different conditions. The most common type is idiopathic pulmonary fibrosis (IPF). IPF affects people who are at least 50 years of age, but can also affect younger people. It often worsens over time, making it difficult to carry out simple daily activities.
If you think you may have pulmonary fibrosis, the healthcare provider will perform a physical examination. During the physical examination, a healthcare provider will listen for any abnormal sounds that occur during breathing. Your healthcare provider will also take blood tests to rule out other illnesses and monitor the disease’s progression.