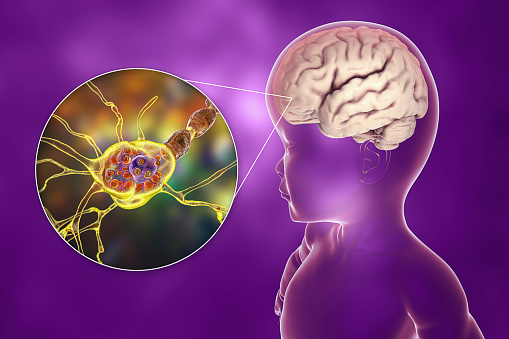
Lysosomal storage diseases are a subgroup of neurodegenerative disorders. These diseases are caused by single gene defects that cause accumulation of substrates in the lysosomes. Although the underlying pathophysiologic mechanisms of these diseases remain unclear, they are believed to result in a progressive neurodegenerative phenotype. Lysosomal storage diseases often affect the central nervous system, primarily neurons, but they can also affect non-neurons.
Is Gaucher disease a lysosomal disease?
The most common form of sphingolipidosis is Gaucher disease, which involves sphingolipid-rich cellular systems in the liver, bone marrow, lymph nodes, and brain. It can also result in neurological, gastrointestinal, and immunological disorders. As a prototype for more than 50 other LSDs, Gaucher disease is also an important research target for a variety of researchers.
The disease manifests in many ways, but the most common is bone pain. When the bones do not receive sufficient blood flow, the bones become weak and brittle. This may lead to arthritis and joint pain. In more severe cases, the bones may die due to lack of blood supply. The disease can also lead to osteoporosis, in which bones do not receive enough calcium, and they can fracture easily.
While a diagnosis of Gaucher disease can be scary, it is important to know that there is hope. Advances in research and treatment can help alleviate symptoms and minimize long-term damage. Working with your healthcare provider is crucial to ensuring the best possible outcome.
Why does lysosomal storage diseases occur?
Lysosomal storage diseases are caused by mutations in the genes that code for the lysosomal enzyme glucocerebrosidase. Because the enzyme is responsible for breaking down and storing complex sugar molecules, improperly functioning lysosomes can damage organs and tissues. There are almost 60 different types of lysosomal storage diseases. The combined prevalence is estimated at 1/4000 to 1/7,000.
The most common lysosomal storage diseases are autosomal recessive, which means that each parent must carry the changed gene. People without such mutations are not at risk. Genetic tests and tissue biopsy are used to diagnose these conditions. Treatments are available to help patients live full and healthy lives.
Although there is currently no cure for lysosomal storage diseases, new therapies are available. These treatments stabilize organ functions and slow disease progression. However, the benefits of these treatments can’t be predicted for individual patients, so it is important to consult with your healthcare provider before participating.
Is Tay-Sachs a lysosomal storage disease?
Lysosomal storage disease (LSD) is a rare genetic disorder in which the body’s cells accumulate toxic materials. These toxic materials damage other cells and organs. People with LSDs lack certain enzymes and a substance that helps the enzymes function. Without these enzymes, the body cannot break down harmful materials, and they build up in the body. These diseases usually show up during pregnancy or early childhood, but can also develop in adults. Treatment is dependent on the type of lysosomal storage disease and underlying cause.
Lysosomal storage disease management involves a multidisciplinary approach. Many treatment strategies can benefit patients with LSD. The most important is patient education. Educating affected families about the disease can help them cope emotionally with the symptoms of the disorder. Support groups are also a helpful resource, enabling people to connect with other individuals facing the same challenges. When symptoms become worse or the results of treatment are slow, patients should see a health care provider. These providers can suggest other treatments to try.
Patients with Tay-Sachs disease may develop muscle weakness, visual difficulties, and neurological problems. A genetic mutation in the HEXA gene leads to an accumulation of glycosphingolipids in the brain and central nervous system. This abnormal buildup in the brain can lead to severe neurodegeneration.
What is Gaucher disease?
There is no specific cure for Gaucher disease, but it can be managed and controlled. Patients need a team of specialists to help them manage the symptoms. The team usually includes a metabolic or biochemical genetics doctor, an orthopedist, and a genetic counselor. Genetic counseling and testing can help families manage the disease and its symptoms. A genetic counselor can answer questions about inheritance, future pregnancies, and tests.
This disease is a genetic disorder characterized by an accumulation of a fatty acid called glucocerebroside in various organs, including the bone marrow, lungs, and brain. The resulting buildup damages organs in various ways, including weakening the bones and causing anemia. The disease may also damage the brain, leading to progressive brain damage.
People with Gaucher disease have low hemoglobin and platelet counts. The disorder affects ninety percent of people. Symptoms may appear in childhood or adulthood. While it is not fatal, it may cause osteoporosis. It also affects the heart and the liver.
Canavan disease is a serious genetic disorder that has no known cure. While the symptoms of this disease last for a long time, support is available for survivors. Research is being conducted to determine how best to treat the condition and help survivors live normal lives. Future treatments may involve gene therapy or vaccines.
Diagnosis of Canavan disease can be made through a variety of tests. The first step is a prenatal blood test, which checks for gene mutations and missing enzymes in the mother’s blood. Another test, known as an amniocentesis, can determine whether the baby has Canavan disease.
Treatment for Canavan disease is tailored to each child’s symptoms and health condition. If swallowing is a problem, feeding tubes may be used to ensure that the child gets enough nutrition. The doctor will also monitor the child’s fluid intake. In severe cases, lithium-based medications may be used to help the child manage seizures.
What is Wagner’s syndrome?
Wagner’s syndrome is a genetic condition that affects connective tissue in the eye. It results in progressive vision loss and is inherited in an autosomal dominant pattern. The disorder is caused by mutations in the CSPG2 gene, which encodes a protein called versican. Some symptoms include changes in the vitreous body of the eye and detachment of the retina. In more severe cases, cataracts may also develop.
Wagner syndrome can also affect the peripheral retina, with peripheral retinal vasculature absent or weak. Other signs include retinal tears, early onset of cataracts, and choroidal atrophy. In 80% of cases, this condition is inherited and requires special testing to be diagnosed. It is caused by a defective gene located on 5q13.4 called Versican.
In 1938, Hans Wagner described 13 family members with the disorder in the Canton of Zurich. In the 1960s, Boehringer and Ricci described another Swiss family. Two more families were described by Jansen in the Netherlands in 1962. However, these families did not have any hearing or joint problems. In 1965, Alexander and Shea reported a family of patients with Wagner syndrome and retinal detachment.
What is Alexander’s disease?
Alexander’s disease is a congenital disorder caused by a gene defect. It is not hereditary, but can be familial. In the early stages of the disease, symptoms are similar to those of multiple sclerosis and Parkinson’s disease. Genetic tests can reveal whether someone has the disorder. Current treatments focus on managing symptoms and slowing the disease’s progression. Clinical trials are also underway to develop new treatments. Children and adults with the disease can participate in these trials.
The age at which the disorder manifests is crucial to a child’s prognosis. In infants, the disease can start as early as the first month of life. In children, it can begin at any age, though it mainly affects young children. Those diagnosed with infantile-onset disease are generally less likely to survive beyond age five.
In infants, the disease is characterized by deposition of Rosenthal fibers, masses of proteins in astrocytes. These proteins inhibit the function of the nervous system. The condition manifests in different clinical forms, depending on the age of the patient. It usually occurs at an early age and has no cure.