Parkinson’s Disease and the Immune System
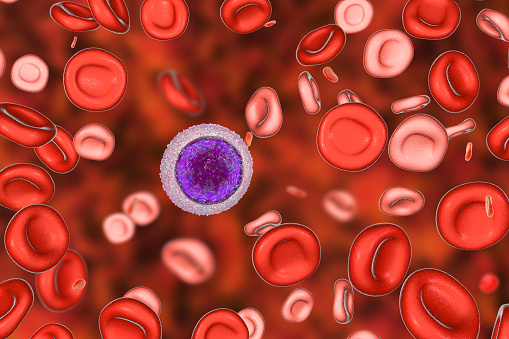
PD, or Parkinson’s disease, is an autoimmune disease that affects the brain. In a study conducted at Columbia University Medical Center, scientists found that a protein called alpha-synuclein accumulates in the Lewy bodies of brain cells that produce dopamine. The aggregation process causes the immune system to respond by producing T-cells.
Parkinson’s autoimmune disease
The discovery that the immune system plays a role in the progression of Parkinson’s disease has important implications for the treatment of the disease. Autoimmunity is when the body’s own immune system attacks healthy cells, tissues, and organs. Several mechanisms contribute to the breakdown of immune homeostasis, which results in an increased level of self-attack and reduced tolerance of autoantigens. In PD, this chronic autoimmune attack is at the core of the pathogenesis of the disease. The first step of the autoimmune attack is inflammation, which is initiated by various immune cells. The resulting damage to these brain cells leads to Parkinson’s disease.
Interestingly, Parkinson’s disease has been associated with an increased production of T cells, which play a role in the immune system. T cells, which are responsible for controlling the production of effector cells, are believed to participate in PD. T cells from people with the disease also express a protein called protein 7 (PD-P). This protein is implicated in the development of the autoimmune response to Parkinson’s disease.
Once believed to be immune-protected, scientists have discovered that neurons are particularly vulnerable to autoimmune attacks. In particular, a 2014 study found that neurons that produce dopamine are susceptible to T cell responses. This is due to the fact that dopamine neurons contain proteins that help the immune system recognize foreign objects. When these proteins are damaged, T cells mistake them for foreign invaders.
Pathophysiological hallmark of PD
The pathophysiological hallmark of Parkinson’s disease (PD) is a buildup of alpha-synuclein, a presynaptic nerve terminal protein. This accumulation may be secondary to an unknown environmental agent or may be a consequence of a genetically-determined disease. This protein causes neuronal degeneration.
Cell loss in the substantia nigra is region-specific, with the lateral ventral tier of the pars compacta most affected. To cause symptoms, at least 50% of the nigral neurons must be degenerated. Autopsy results show a reduction of up to 80% in the number of nigral neurons in the brain.
Degeneration of brain cells results in loss of dopaminergic neurons, a key factor in the underlying pathophysiology of PD. This loss of neuronal activity disrupts neurotransmitter systems in different parts of the brain, including subcortical areas. These changes are thought to contribute to the psychiatric and cognitive symptoms of PD.
PD is also associated with neuronal loss in the medulla, including the dorsal motor nucleus and the olfactory bulb. This may explain changes in smell in patients with the disease. Additionally, the sympathetic nervous system, which controls movement and sensation, may be involved. This involvement can explain why patients with PD struggle with urination.
Tau may also be a key factor in PD pathogenesis. It may be involved in the deposition of a-Syn and the deterioration of excitatory synapses. This mechanism may provide new targets for early diagnosis and treatment of PD.
Contributing factors to pathogenesis
While the causes of Parkinson’s disease are unknown, researchers believe that inflammation is an important contributing factor. Postmortem studies of PD brains have shown accumulation of alpha-synuclein, increased expression of major histocompatibility complex II (MHC-I), and degeneration of dopaminergic cells in the substantia nigra. More recent findings have also indicated that T-cells recognize a-synuclein epitopes.
Genetic studies have identified several genes as contributing factors to parkinson’s autoimmune disease. Two of these genes, Parkin and PINK1, encode proteins with functions associated with immune responses. These genes affect the brain’s immune response, and their mutations result in early dopaminergic neuron degeneration in patients. Additionally, both parkin and PINK1 cause abnormal expression of immune-modulatory genes in the striatum.
Neuroinflammation, genetics, and the innate and adaptive immune systems are implicated in the pathogenesis of PD. Autoantibodies, which are antibodies against proteins that trigger autoimmune responses, contribute to parkinsonism. Some people with autoimmune diseases are more likely to develop PD.
HLA class I and HLA class II are also associated with the development of PD. However, it is not known which of these genes are responsible for the development of the disease. There are numerous other risk factors, but these two genes may play a major role in the development of the disorder.
Complications
One of the most common complications of Parkinson’s autoimmune disease is an increased risk for infections. People with Parkinson’s disease have increased levels of immune cells in the blood. This is an interesting discovery that offers hope for better treatment. Although it is still a mystery how these immune cells influence the progression of the disease, the results suggest that they are linked.
The disease can also cause increased blood sugar levels. This condition is caused by the body becoming resistant to the hormone insulin, which helps transport glucose from the blood to the body’s cells and provides energy. Diabetes can cause several health complications, including Parkinson’s disease. The symptoms of these illnesses are similar and can be confusing.
Researchers at the La Jolla Institute for Immunology are investigating the role of the immune system in Parkinson’s disease and its complications. They have discovered evidence that certain T cells mistakenly target brain cells and contribute to the progression of the disease. Their findings could lead to better diagnostics and treatments for patients with Parkinson’s. But more research is needed to find out the precise role of autoimmunity in the disease.
Researchers have found that patients with recent outbreaks of HIV, Epstein-Barr virus, Japanese encephalitis, Coxsackie virus, and Western Equine virus are at increased risk for Parkinson’s disease. Infection with these viruses can damage the basal ganglia, which control movement. Once these cells are damaged, Parkinson’s disease can set in.
Genetics
Researchers have linked Parkinson’s disease to the immune system, and their findings could lead to better treatments. The researchers studied 2,000 patients and healthy individuals, assessing various environmental, genetic, and clinical factors. Some participants were followed for two decades. They found an association between the disease and the HLA region, a region of the human genome with many genes related to the immune system. The findings encourage further investigation into the role of infection, inflammation, and autoimmunity in Parkinson’s disease.
Two HLA loci, Hicks AA and Jonsson T, were associated with Parkinson’s disease risk. Another locus associated with the disease is chromosome 4p. The study found that mutations in these loci may contribute to the risk of Parkinson’s disease.
The gene SNCA is responsible for producing the protein that triggers the disease. It is thought that 15 percent of those with Parkinson’s disease have a family history. The genetic mutations that cause familial cases of the disease are associated with the PINK1 or the SNCA gene. However, the interplay between these genes and the risk of Parkinson’s disease remains poorly understood.
LRRK2 is also implicated in Parkinson’s disease. Patients with this mutation have an increased kinase activity. This is associated with both early and late onset symptoms.
Environmental factors
Environmental factors play an important role in the development of Parkinson’s disease. Research shows that long-term exposure to solvents such as trichloroethylene may be associated with the development of the disorder. Moreover, organic pollutants like polychlorinated biphenyls (PCBs) have been found in the brains of people with Parkinson’s. Research on these environmental factors continues.
In addition to the environmental factors, other factors may contribute to the development of the disease. These include pathogenic infections, head trauma, dietary factors, drugs and supplements, air pollution, and physiological stressors. Environmental factors are complex, so the exact relationship between environmental factors and disease is still not clear. However, studies have shown that gene-environment interactions can contribute to the disease phenotype.
The incidence of PD varies considerably around the world. Recent estimates indicate that PD is the fastest growing neurological disease in the world, with heavy societal and economic costs. In 1990, there were an estimated 2.5 million people with the disease. By 2015, that number had risen to 6.2 million. This number is expected to double again by 2040 due to population aging. There are also other factors that may drive the prevalence of the disease higher. For instance, PD is growing in the newly industrialized regions of the world.