Is Lyme Disease an Autoimmune Disease?
There are several reasons that it is hard to determine if Lyme disease is an autoimmune disease, but one major reason is that it suppresses the immune system. Antibiotics like Methotrexate and Humira suppress the immune system, making Lyme disease more difficult to treat. In addition, doctors are often unwilling to try new treatments due to their arrogance and ignorance.
Lyme disease is an autoimmune disease
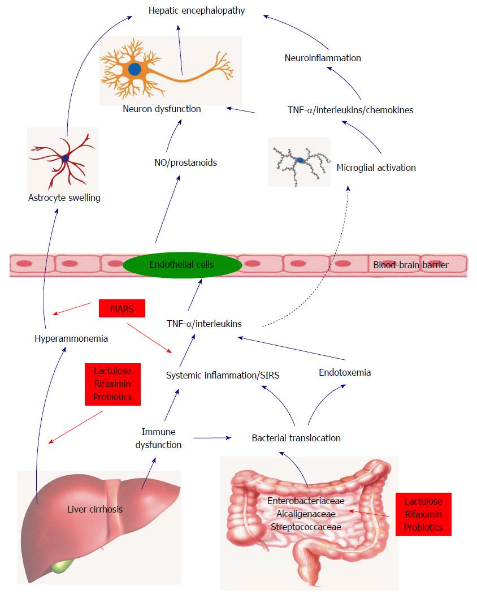
Unlike most other diseases, Lyme disease is an autoimmune disease, which means that the immune system attacks healthy cells. The body’s antibodies attack body parts that resemble the bacteria that causes the disease, causing damage to healthy tissues. Lyme disease is caused by a bacterium that hides inside body cells, called Borrelia burgdorferi. When this bacteria infects a person’s body, it triggers a response in the body that causes rashes and joint swelling. While traditional treatments for Lyme disease are inconsistent and often misdiagnosed, current research is helping doctors understand the condition better.
Some of the symptoms of Lyme disease are similar to other autoimmune diseases, like rheumatoid arthritis. However, there are some key differences that distinguish the two types of autoimmune diseases. Lyme disease antibodies are usually less potent than antibodies to other diseases, such as lupus or rheumatoid arthritis.
Currently, the CDC reports around 30,000 new cases of Lyme disease each year, although the actual number is probably closer to 476,000. Although Lyme disease is not considered an autoimmune disease, it may trigger an autoimmune response in the body, causing certain symptoms of an autoimmune disorder.
While more research is needed to determine a link between Lyme disease and autoimmune diseases, the existing evidence is helpful for doctors and patients. The following article will discuss some of the similarities between Lyme disease and autoimmune diseases. It will also highlight some key points to consider when trying to diagnose Lyme disease.
Undiagnosed Lyme disease can lead to long-term symptoms. The disease can recur even with antibiotics. Many people with untreated Lyme disease are not diagnosed until it is too late. Moreover, the longer Lyme disease goes untreated, the more neurotoxins the body produces and the more damage it causes to cell tissue. Therefore, it’s critical to get medical advice immediately.
While antibiotics are effective in treating Lyme disease, they also suppress the immune system, making it difficult to cure. The use of a combination of antibiotics such as Humira and Methotrexate is not always the best treatment. Antibiotics can also cause a variety of autoimmune diseases in patients.
Lyme disease is caused by a bacterium that infects human cells. It can spread to other parts of the body, causing serious health issues. Its symptoms include muscle pains, numbness, and fever. Some people may not show any symptoms at all.
There are no treatments that can completely cure the disease. In some cases, it may take a few years for symptoms to appear. The symptoms can also become chronic, requiring several years of treatment. The doctors must make a proper diagnosis and follow up. The treatment must be individualized to address the cause of the disease.
It’s important to understand that autoimmune diseases can affect any part of the body. Some of these diseases can cause the immune system to become overactive, attacking its own tissues. For example, people with a tick bite may develop dermatomyositis, which is an inflammatory disease characterized by muscle weakness.
Lyme disease mimics rheumatoid arthritis
Lyme disease can mimic rheumatoid arthritis and can cause joint pain and swelling. It typically affects the knees, but can also affect other joints. This disease is triggered by infection elsewhere in the body, such as a bacterial infection or sexually transmitted infection. Although there is no known cure for Lyme disease, anti-inflammatory drugs can help relieve symptoms.
Antibiotic-refractory Lyme arthritis has an autoimmune component, and is characterized by a dysregulation of CD4+ T regulatory cells and the presence of some HLA-DR alleles. Patients often experience arthritis in one joint, and it usually clears up on its own after a short course of antibiotic treatment.
Arthritis is a late symptom of Lyme disease and often occurs months after tick bite. Patients may have a history of erythema migrans but may not experience arthritis. Arthritis typically manifests with intermittent joint swelling and persistent joint pain. Patients with persistent synovitis may require disease-modifying antirheumatic drugs, anti-inflammatory drugs, and even synovectomy.
Reactive arthritis is a seronegative spondyloarthropathies that usually appear within a month of an underlying disease. Symptoms of reactive arthritis occur in the same joints as rheumatoid arthritis, but the inflammation is localized and does not involve the whole body.
The symptoms of Lyme arthritis can be managed using oral antibiotics. If the symptoms persist, the doctor may prescribe an intravenous antibiotic. The treatment of Lyme arthritis may include doxycycline or amoxicillin. However, only a small proportion of patients will respond to oral antibiotics.
Anti-inflammatory drugs are the most common treatments for rheumatoid arthritis. Patients may be prescribed non-steroidal anti-inflammatory drugs, steroid injections, or physical therapy. Surgery may also be necessary in rare cases. It is important to note that a misdiagnosis of RA and Lyme disease can be very expensive and even life-threatening.
Because rheumatoid arthritis has many symptoms, it can be difficult to diagnose in the early stages. Nearly half of the people diagnosed with RA actually have another condition. Many other ailments have similar symptoms. For instance, Lyme disease and gout may have some similarities to RA, which can cause confusion.
During the early stages of Lyme arthritis, patients may use over-the-counter pain relievers to manage their symptoms. In later stages, treatment may involve a 28-day course of antibiotics, such as amoxicillin and doxycycline. Once the infection has cleared, the symptoms of Lyme arthritis will subside. Surgery is another option for resolving Lyme arthritis.
Rheumatoid arthritis is a serious chronic disease that can result in joint damage and pain. Treatment for rheumatoid arthritis is available, but the disease cannot be cured. If you have symptoms of either disease, it is important to see a doctor to diagnose the underlying cause. A doctor can help you develop a treatment plan and recommend medications if necessary.
Lyme disease evades antibiotic treatment
Antibiotics can kill persister cells in Lyme disease, but the bacteria that causes the disease also has the ability to evade them. A group of researchers from Northeastern University have recently discovered that the bacterium responsible for the disease forms a type of specialized cell called a persister cell, which is resistant to many common antibiotics. The good news is that two approaches to eradicating persister cells have been proposed.
Antibiotics have been shown to be effective in treating Lyme disease, but the symptoms can be long-lasting, resulting in a high risk of long-term health problems. The CDC estimates that nearly half of all new cases of Lyme disease are treatable with antibiotics. Approximately 10 to 20 percent of people treated with antibiotics develop long-term symptoms of the illness, including joint/muscle pain, severe fatigue, and neurologic problems. As a result, only a small percentage of National Institutes of Health dollars are dedicated to the development of effective treatments for Lyme disease.
Researchers are working on a new approach to treating Lyme disease. The first step in this approach is to identify the proteins that Lyme bacteria use to protect themselves from antibiotics. Antibiotics kill the good bacteria in your digestive system, so it’s important to take probiotics as soon as you’re infected. A second course of antibiotics may be necessary for late-stage infections. However, antibiotic treatment beyond one repeat round is not effective and may lead to serious complications.
Antibiotics are most effective if they are administered within three months of the tick bite. However, if they are not administered within this time frame, the bacteria may continue to survive in your body and evade antibiotics. Antibiotics can help cure the infection, but the bacteria often evade them and remain dormant, causing the symptoms to appear years later.
Antibiotics cannot cure all the symptoms of chronic Lyme disease, but they can help reduce the inflammation that occurs in the body. Antibiotics can also help reduce tissue damage and speed up healing. This is why they are a critical part of the treatment of chronic Lyme disease. The CDC reporting criteria for the diagnosis of Lyme disease are largely too restrictive, and many patients are diagnosed late, often in the tertiary stage.
Although the scientific understanding of the pathogenic bacteria responsible for Lyme disease is not complete, some basic facts are well known. The bacterium responsible for Lyme disease is a spirochete called Borrelia burgdorferi. The bacterium can infect any part of the body. If untreated, the disease can spread to the joints, heart, and nervous system.
Patients who have been treated with antibiotics shortly after the infection will recover without any problem. However, patients who have persistent symptoms should seek medical advice to determine whether they need antibiotic treatment. The use of antibiotics may result in a rash that lasts for a few days.