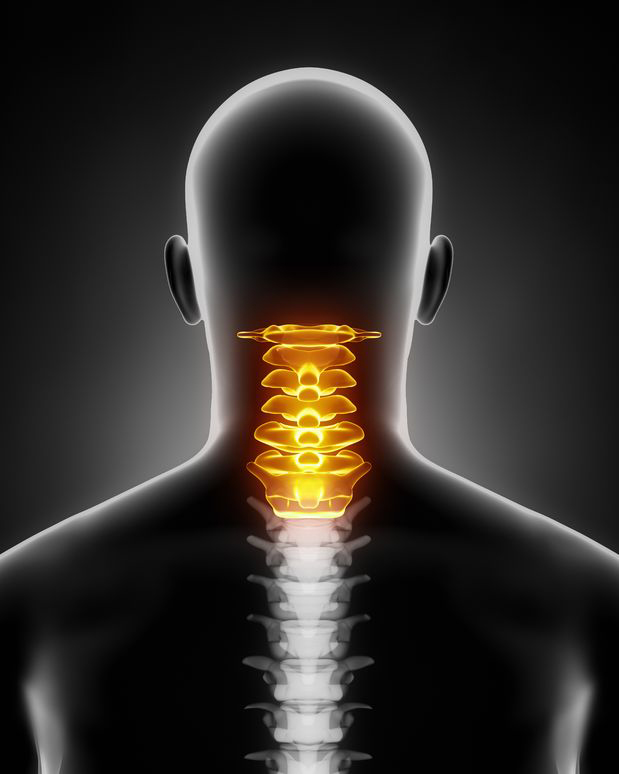
Cervical Degenerative Disc Disease, ICD-10 Revision
What is cervical degenerative disc disease?
The International Classification of Diseases, 10th revision, is used to classify health conditions. During the study period, 1659 cases of cervical disc disorders were diagnosed. Most of these conditions are classified under general code M50, including subtypes such as M50.1 and M50.2 (cervical disc disorder with radiculopathy). The number of cases of M50 cases increased between 2011 and 2013, but then decreased between 2014 and 2015. The ICD-10 is a comprehensive, universal classification system, and is the best available for diagnosing medical conditions.
Disc disorders are common in orthopedic practices. As a result, medical coding for these conditions must be more specific than ever. The new ICD 10 coding system classifies these conditions according to their location within the cervical spine. In addition, these codes require an indication of either radiculopathy or myelopathy, allowing for more detailed reporting.
While most patients with cervical degenerative disc disease undergo imaging studies and physical examinations to determine their causes, these studies do not show a definitive answer to the question of whether the condition is indeed caused by degenerative discs. Disc degeneration is a gradual process involving intervertebral discs. The condition results in loss of normal function and structure. It may be a result of aging or repetitive motion stress.
What is the ICD-10 code for cervical disc C5 C6?
Cervical disc disorders are among the most common conditions seen in orthopedic practices. As such, they need accurate orthopedics medical coding in order to be properly reported. Traditionally, cervical disc disorders have been classified based on the region of the cervical spine. However, the new coding system requires more specific data, including an indication of radiculopathy or myelopathy.
In the study period, 1659 cases of cervical disc disorders were diagnosed. Of these, a general code M50 classified the vast majority of them. The most common subtype was M50.1 for cervical disc disorder with radiculopathy. In addition, M50.2 included other cervical disc displacements. The number of cases increased in the years 2011-2013, but then gradually declined between 2014-2015.
The diagnosis of cervical degenerative disc disease is typically diagnosed through a physical examination and imaging studies. Cervical disc disease is a serious problem that can cause severe pain. It requires a thorough examination by a medical professional, and it is not uncommon for pain to radiate to the arm. In addition to a physical examination, the diagnosis may require special diagnostic tests such as CT scans.
What are the 4 stages of degenerative disc disease
The four stages of cervical degenerative disc disease are accompanied by an array of symptoms. Some of these symptoms are a result of pain, while others are neurological. Most people with this disease undergo nonoperative treatment, in the hopes that their symptoms will improve over time. However, the more advanced stages of the disease can lead to significant limitations in function and mobility.
In the initial stages of the disease, the cervical disc offers less cushioning to the spinal column. This makes it prone to tears and cracks. It also lacks direct blood supply. Instead, it draws nutrients and metabolites from the adjacent vertebrae. When a disc tears, it cannot heal itself, and the scar tissue that develops becomes weak. Cervical degeneration is a degenerative process that affects everyone at some point.
Cervical disc disease can lead to poor quality of life and disability. Consequently, it’s vital to recognize early symptoms of the condition, and to get a correct diagnosis. The best way to do this is to work with your primary care physician. Not only should they be trained to recognize the signs of cervical disc disease, but they should also have a good referral system.
What vitamins help degenerative disc disease?
Cervical degenerative disc disease (CDD) is a common problem that can be diagnosed using X-rays or MRIs. People who have disc degeneration will usually experience some level of pain, though the level of pain varies significantly. It is often determined by where the affected disc is located and the amount of pressure it puts on the spinal column and nerve roots.
Does stretching help degenerative disc?
Disc degeneration is a common cause of neck and back pain. It affects approximately 30 million people each year. Symptoms vary depending on the location of the affected disc. If it is in the lower back, the patient can experience pain in the lower back, buttocks, and thighs. Pain may also radiate to the arms and fingers. The condition can make sitting, bending, and standing for long periods of time difficult.
If the pain persists, your doctor may suggest a surgical procedure to relieve the pressure on the nerve. However, in many cases, nonsurgical treatments can relieve the pain and make it manageable. The doctor may prescribe spinal injections or physical therapy if the symptoms are severe.
Degenerative disc disease is a common condition that affects people of all ages. While there is no cure for this condition, it is a common part of aging. The spine’s discs thin as we age, leaving them vulnerable to injury. As these discs become weaker, the pain can increase and get worse when we sit or bend.
Can chiropractor help degenerative disc disease?
The ICD-10 transition is a daunting task for medical coders, especially those working for hospitals or in general practices. However, it is less intimidating for chiropractors, who will need to familiarize themselves with specific chiropractic codes. While ICD-9 had some limitations, ICD-10 offers more detailed diagnostic codes that will reduce claim denials and ensure accurate reimbursement.
To code for a patient with a cervical degenerative disc disease, a chiropractor will need to know the appropriate diagnosis code. Usually, a chiropractor will use the code for cervicalgia or lumbago. Non-specific codes simply state that the patient is experiencing back or neck pain but don’t tell them why. In contrast, ICD-10 codes will tell you whether a condition is chronic or acute and whether it’s on the right or left side of the body. In addition, injury codes will contain the seventh character known as extension.
Patients with degenerative disc disease typically experience lower back pain in the neck. Depending on the location of the affected disc, pain may extend from the lower back down to the buttocks or thighs and legs. Pain may also result from the compression of the nerve roots in the cervical region.
What can you not do with a DDD?
Intervertebral discs in the cervical region degenerate over time due to repeated stress and strain. Symptoms of this condition often begin with a stiff neck and require imaging studies to diagnose. ICD-9 medical coding had only one code for this disorder, but the new ICD-10 system has four different codes.