Is Atypical Kawasaki Disease Fatal Or Treatable?
If you have been diagnosed with atypical Kawasaki disease, you may be wondering if the condition is fatal or treatable. Read on for information about the symptoms and treatment of this condition, as well as its survival rate. You should also learn how to prevent the disease, and how to keep yourself healthy while living with it.
How is atypical Kawasaki diagnosed?
The symptoms of Kawasaki disease are not the same in all children and parents need to know which signs and symptoms to look for. A fever higher than 102.2 degrees Fahrenheit is one of the most common signs, but the symptoms may not occur at the same time. If the symptoms do not go away after a few days, parents should contact their health care provider. Early diagnosis of Kawasaki disease is important because it can damage the heart muscle and coronary arteries if not treated quickly.
Kawasaki disease can be diagnosed by a cardiology team that will perform a physical examination and take lab tests. An echocardiogram and C-reactive protein (CRP) are two of the main tests used to diagnose this disease. ESR and platelet count are the other key tests used to diagnose this disease. Once the diagnosis is made, a treatment plan will be recommended.
AHA-recommended diagnostic criteria for the diagnosis of incomplete Kawasaki disease include three or more of the four principal signs. Some pediatricians use the Japanese criteria and occasionally encounter patients with less than four principal symptoms. However, these criteria are too narrow.
What is the survival rate of Kawasaki disease?
There is a low mortality rate of Kawasaki disease in hospitalized children. Most deaths occur as a result of cardiac sequelae. Peak mortality occurs between fifteen and forty-five days after fever onset, and is associated with coronary artery vasculitis and marked hypercoagulability. Despite the low mortality rate, the disease can damage the heart and lead to complications. It can lead to coronary artery aneurysms, which increase the risk of blood clots and heart attacks. Children with Kawasaki disease should be properly evaluated and treated to avoid these risks.
The diagnosis of Kawasaki disease is made through a detailed history and physical exam. The patient may also have an echocardiogram, an ultrasound of the heart. The child will then receive treatment based on the symptoms and lab results. The prognosis for a child with Kawasaki disease is not known for sure.
Children with Kawasaki disease require a team approach, including a pediatric cardiologist and an infectious disease specialist. A pediatric rheumatologist may also be consulted. As children with Kawasaki disease are at high risk of developing coronary artery aneurysms, therapy must begin as soon as possible. Treatment usually involves high-dose IVIG given over ten to twelve hours and high-dose aspirin given four to eight times a day.
Is Kawasaki a lifelong disease?
Although Kawasaki disease is a chronic condition, it is treatable. Treatment usually involves long-term aspirin dosing and blood-thinning medications. It may also require certain procedures. Patients with Kawasaki disease should avoid certain lifestyle factors that increase the risk of heart attacks, such as smoking, obesity, and high blood cholesterol. In some cases, Kawasaki disease may require a lifetime of care, but in the majority of cases, treatment can eliminate the risk of a heart attack.
Kawasaki disease is rare, and it typically affects infants and young children. It can lead to a high fever and inflammation of the heart muscle. It also may cause an irregular heartbeat and aneurysms. Although it is rare in adults, it is one of the leading causes of acquired heart disease in children in the United States.
If your child has Kawasaki disease, you should consult a cardiology doctor. These doctors will examine your child and perform a thorough physical exam and ECG to confirm the diagnosis. Then, they will likely perform an echocardiogram, which is an ultrasound of the heart. Once they have diagnosed your child’s Kawasaki disease, they will prescribe appropriate treatment.
How do you get Kawasaki disease?
Atypical Kawasaki disease is a rare but potentially serious condition that causes inflammation of the blood vessels. It often affects the coronary arteries. This inflammation can lead to a condition called coronary artery aneurysm. These aneurysms are balloons that form in the wall of a blood vessel. The good news is that treatment is available and can prevent the development of an aneurysm. However, treatment should be started as soon as possible.
The first step in the treatment of Kawasaki disease is to diagnose it. The best time to do so is during the first 10 days after infection. After discharge, your child will need to take low-dose aspirin every day for six to eight weeks. They will also be monitored by a cardiologist to ensure the condition is under control.
In most cases, this disease affects children younger than 5 years of age. The symptoms generally subside after a few weeks, but in some cases, it may take longer. If you notice that your child’s symptoms are severe, you should visit your GP as soon as possible.
What are the 3 phases of Kawasaki disease?
The diagnosis of Kawasaki disease is based on a combination of certain symptoms and clinical findings. These include a persistent fever, elevated inflammatory markers, and compatible echocardiographic findings. Infants with unexplained fever over seven days should have blood tests for inflammatory markers, including C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR). Patients with Kawasaki disease may also need to undergo surgical procedures to restore arterial flow, including a coronary artery bypass graft or percutaneous coronary intervention.
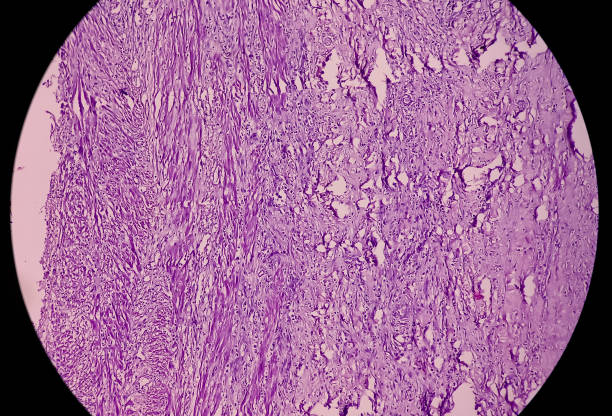
While Kawasaki disease is rare in adults, it is a leading cause of acquired heart disease in children. This autoimmune disease is caused by an unidentified infectious pathogen, which causes a generalized vasculitis in the heart. Although the disease can be treated with intravenous immunoglobulin (IVIG), some cases can develop resistance to the therapy. Fortunately, treatment with IVIG may reduce the risk of coronary artery aneurysms. However, many children with untreated Kawasaki disease may develop coronary artery abnormalities that eventually lead to thrombosis and segmental stenosis.
The underlying cause of Kawasaki disease is unknown, but it is suspected to be a viral infection. The virus may enter the body through the mucosal surfaces of the lung. Kawasaki disease outbreaks are seasonal, similar to other respiratory infections, peaking in spring and winter.
What viruses cause Kawasaki?
Atypical Kawasaki disease is the result of an inflammatory reaction in the body. This reaction is the result of the immune system’s type III hypersensitivity reaction to viruses with large surface area and high replication rates. The symptoms of atypical Kawasaki disease can include fever, diarrhea, and fatigue.
If you suspect your child has Kawasaki disease, he or she will need to see a doctor right away. The symptoms of the illness are similar to those of multisystem inflammatory syndrome. Children with COVID-19 are at increased risk for this condition. Fortunately, most children recover without any long-term effects.
Although the COVID-19 pandemic began in early 2020, it is still unknown how widespread the virus is or what the trigger is. The recent reports that describe a hyperinflammatory response to COVID-19 in children have generated a lot of media attention.
Is Kawasaki disease an autoimmune disease?
Although the underlying cause of Kawasaki disease is unknown, it is believed to be an inflammatory response to multiple infectious agents. Plasma cells containing IgA are infiltrated into the respiratory tract, with the upper airways acting as a portal of entry. The triggering agent is not entirely clear, but recent findings suggest it may be an environmental toxin or antigen. However, a definitive answer to this question will be available only after the precise identification of the aetiological agents.
Recent studies indicate that the ITPKC pathway plays a critical role in the development of Kawasaki disease. In vitro, an impaired ITPKC gene results in increased Ca2+ flux and IL-1b levels. In vivo, Kawasaki disease is associated with an impaired B cell maturation process and poor humoral immune responses.
Kawasaki disease is a potentially deadly autoimmune disease that affects the blood vessel wall. It can lead to a heart attack, especially if it develops late in life. The disease causes high fever and inflammation in the blood vessels. Although most children will recover, a few patients may develop aneurysms and heart failure.
How serious is Kawasaki?
Atypical Kawasaki disease is a serious heart disease that affects young children. It begins suddenly and causes the walls of the blood vessels to swell. In time, this inflammation can lead to damage to the coronary arteries. These vessels provide the heart with oxygen. Symptoms may include fever, swollen fingers and toes, and red eyes. Although the disease is highly treatable, it is important to seek treatment immediately.
Children with Kawasaki disease should be evaluated by a pediatric cardiologist and other specialists to determine the cause of the condition. The doctors will conduct a history and physical exam and may order certain tests. These tests can include an electrocardiogram, which measures heart rate, and an echocardiogram, which uses sound waves to create images of the heart. Once the cause of the condition is determined, treatment will be prescribed.
Symptoms of Kawasaki disease can mimic those of another condition called multisystem inflammatory syndrome. However, the symptoms don’t all occur at the same time. As a result, if a child develops symptoms of Kawasaki disease, they should see their doctor right away. Treating the condition early is important because it can prevent damage to the heart muscle and coronary arteries.